Wellfleet Student plans are designed with the goal of member satisfaction, by delivering the right care, at the right place, for the right price. Through a partnership with Cigna, Wellfleet gives its student members access to over 1.2 million providers at over 6,000 facilities nationwide. In addition to having a great network partner, we have a passionate internal team that works tirelessly for our members. This includes customer service, a quality assurance department, and provider and clinical team, with oversight from our Chief Medical Officer.
Wellfleet’s Payment Integrity team
Our Payment Integrity Team works closely with network partners and vendors to ensure our members have access to high-quality, in- and out-of-network care. As faithful stewards to our members, the team works with providers on a case-by-case basis, to help reduce their out-of-pocket responsibility and retain costs for the health plan.
Not satisfied with business as usual
When high-dollar claims come into Wellfleet, there are several internal teams that review them. This is to ensure the bill is appropriate for the care provided. The steps in their process ensure proper evaluation, to provide the fairest outcome for the member and the plan. Most times these high-dollar claims are appropriate, and the approval is seen as business as usual. However, some raise flags based on things like billing, coding, or prior treatments.
Newborn starts a family and billing scrutiny
Wellfleet provides coverage for hundreds of student members who are starting a family each year. From prenatal appointments and ultrasounds, to pre- and post-delivery care, we help parents prepare for the anticipated and unexpected as they welcome their newborns into the world.
In this instance, a student member welcomed their new baby via a planned cesarian section and spent three days in the hospital before returning home.
While this seemed like a normal birth, our Payment Integrity Team was caught off-guard when reviewing the billing, as it included billing codes associated with major problems post-birth.
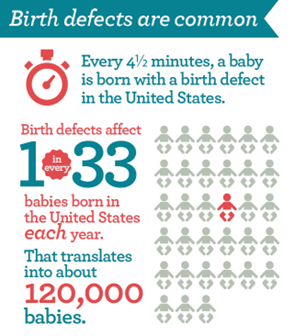
Now a newborn experiencing problems post-birth isn’t unusual. In fact, thousands of birth defects exist. According to CDC statistics, one in every 33 babies will experience a birth defect, with some of the most common defects being heart problems, cleft lip and palate, and Down Syndrome.1
When these conditions are present, the medical records will include associated factors, tests, and procedures that help with follow-up care, and confirmation on billing. Here, no notes or additional procedures were present in the medical records. So, the lack of underlying information prompted the Payment Integrity Team to start further investigation.
Unsupported bill coding leads to big plan savings
After a deeper dive into the medical records, the team could not find any evidence to support the billing codes. From their work, they determined that there was an error in the submission and communicated with the facility to correct the billing.
By correcting the billing to reflect a normal birth, the Payment Integrity Team was able to save the school’s plan more than $83,000! This also resulted in the student member saving more than $5,000, in out-of-pocket costs.
Don’t miss another great savings story! Sign up for our monthly clinical newsletter and get member savings stories in your inbox with other great Wellfleet Student happenings.
Resource
1 March of Dimes. (n.d). Birth Defects and Your Baby. Retrieved on February 10, 2025, from https://www.marchofdimes.org/find-support/topics/planning-baby/birth-defects-and-your-baby