Wellfleet Student plans are designed with the goal of member satisfaction, by delivering the right care, at the right place, for the right price. Through a partnership with Cigna, Wellfleet provides its student members access to more than 900,000 providers at more than 6,000 facilities nationwide. In addition to having a great network partner, we have a passionate internal team that works tirelessly for our members. This includes customer service, a quality assurance department, and provider and clinical team, with oversight from our Chief Medical Officer.
Wellfleet’s Provider Network team
Our Provider Network team works closely with network partners and vendors to ensure our members have access to high quality, in- and out-of-network care. As faithful stewards to our members, the team works with providers on a case-by-case basis, to help reduce their out-of-pocket responsibility and retain cost for the health plan.
Not satisfied with business as usual
When high-dollar claims come into Wellfleet, there are several internal teams that review them. This is to ensure the bill is appropriate for the care provided. The steps in their process ensures proper evaluation, to provide the fairest outcome for the member and the plan. Most times these high-dollar claims are appropriate, and the approval is seen as business as usual. However, some raise flags based on things like billing, coding, or prior treatments.
Cutting through inaccuracies
A student member went to the hospital with abdominal discomfort. Doctors attributed the pain to abdominal adhesions caused by an abdominal surgery the member had a few months prior.
Abdominal adhesion are bands of scar-like tissue that form inside the abdomen. They are common and often develop after an abdominal surgery. The bands end up forming between two or more organs or between organs and the abdominal wall. They can twist, pull, or compress the intestines and other organs in the abdomen, causing discomfort and serious complications associated with intestinal obstruction.
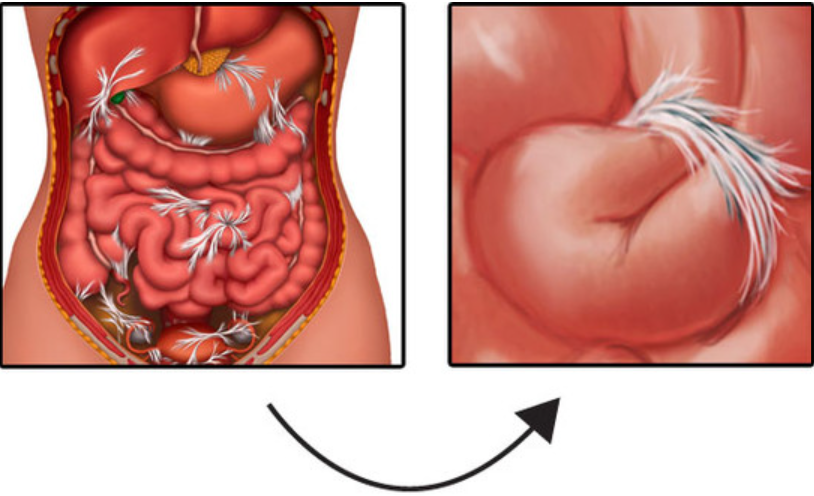
Doctors confirmed the presence of abdominal adhesions, fortunately without obstruction. So, they scheduled a laparoscopic surgery the next day to remove them. The surgery was a success, and the student member was feeling well enough to return home the following day.
When the billing was received by the payment integrity team, they found coding related to symptoms and procedures that didn’t align with the principal diagnosis and procedure. Among other things, it included a diagnosis for non-celiac gluten sensitivity and obstruction – both were inaccurate.
In working with the provider to apply the appropriate charges, they helped save the plan more than $62,000 and the member more than $6,000 in out-of-pocket fees.
Visit https://wellfleetstudent.com to learn more about Wellfleet Student’s commitment to our clients and members.