Wellfleet Student plans are designed with the goal of member satisfaction, by delivering the right care, at the right place, for the right price. Through a partnership with Cigna, Wellfleet provides its student members access to more than 900,000 providers at more than 6,000 facilities nationwide. In addition to having a great network partner, we have a passionate internal team that works tirelessly for our members. This includes customer service, a quality assurance department, and provider and clinical team, with oversight from our Chief Medical Officer.
Wellfleet’s Provider Network team
Our Provider Network team works closely with network partners and vendors to ensure our members have access to high quality, in- and out-of-network care. As faithful stewards to our members, the team works with providers on a case-by-case basis, to help reduce their out-of-pocket responsibility and retain cost for the health plan.
Not satisfied with business as usual
When high-dollar claims come into Wellfleet, there are several internal teams that review them. This is to ensure the bill is appropriate for the care provided. The steps in their process ensures proper evaluation, to provide the fairest outcome for the member and the plan. Most times these high-dollar claims are appropriate, and the approval is seen as business as usual. However, some raise flags based on things like billing, coding, or prior treatments.
Correcting back and billing pains
A student member was experiencing chronic back pain due to scoliosis, which is a sideways curvature of the spine – and sought help to alleviate it.
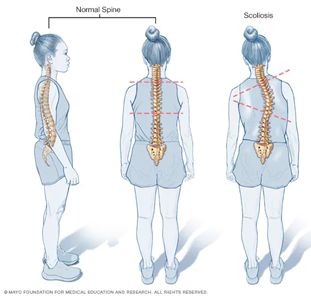
The member was able to work with a quality, in-network doctor to discuss the symptoms and identify the best treatment for her condition. They agreed on a spinal fusion.
Spinal fusion is an operation where a surgeon puts pieces of bone or a similar material between bones in the spine to grow together, or fuse. The goal of the surgery is to help lessen the curve in the spine and reduce recurring pain. The surgery can take several hours, and patients typically have a four-to-seven-day recovery at the hospital.
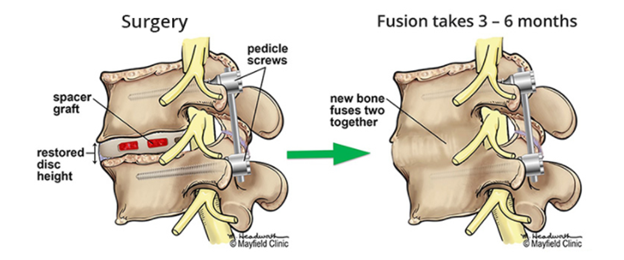
The surgery was a success and the student member returned home to start healing and begin physical therapy.
Weeks later, the medical bill was received by Wellfleet and provided to the Payment Integrity Team for review. Initially the claim looked fine, but coding noted complications during surgery. So, the team began to scrutinize the file, and was unable to find anything abnormal in the process. Rather, it was a typical surgery and recovery. Upon discussion with the provider, they determined that complications were added in error and agreed to remove the additional charges.
The work of the Payment Integrity Team saved the client more than $43,000 dollars and the student member more than $4,000 in out-of-pocket fees!
Visit wellfleetstudent.com to earn more about Wellfleet Student’s commitment to our clients and student members.